The facial nerve takes center stage in the realm of rhytidectomy, marking it as the pivotal nerve to navigate with utmost care.
Advertisement
Governing all facial muscles, any harm incurred can result in temporary or enduring effects such as drooping, twitching, or paralysis.
Given its extensive branching across the face, surgeons prioritize cautious dissection throughout the procedure.
To mitigate risks, surgical experts utilize a spectrum of techniques. Nerve monitors prove invaluable, aiding in real-time assessment.
Meticulous identification of anatomical landmarks is another crucial step, ensuring precision. Additionally, employing blunt dissection techniques contributes to a safer surgical journey.
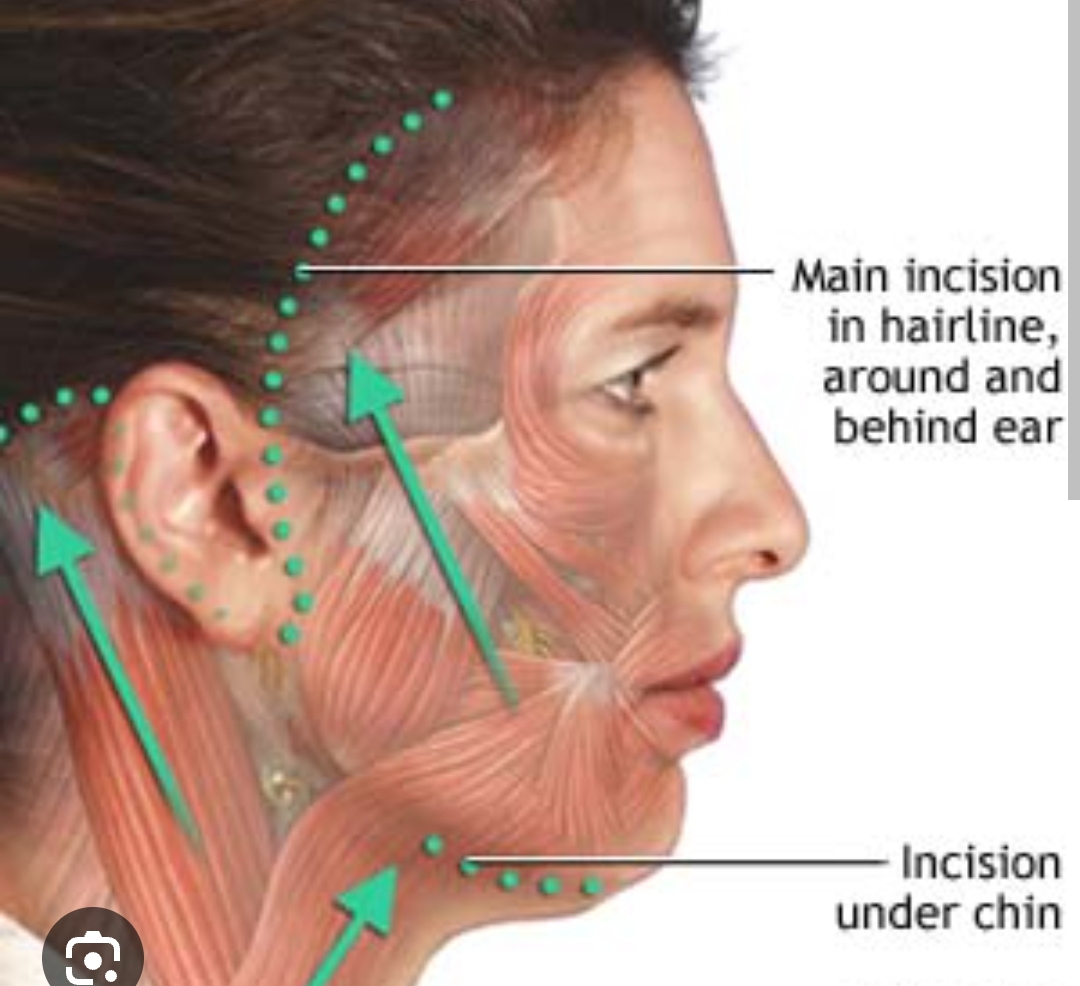
Photo via Drugs.com
While peripheral nerves like the great auricular nerve in the neck may be impacted, the facial nerve stands out as the primary concern.
Advertisement
Its pivotal role in orchestrating facial movement and expression underscores the significance of safeguarding it during the intricate dance of a rhytidectomy.
What nerve is injured in rhytidectomy?
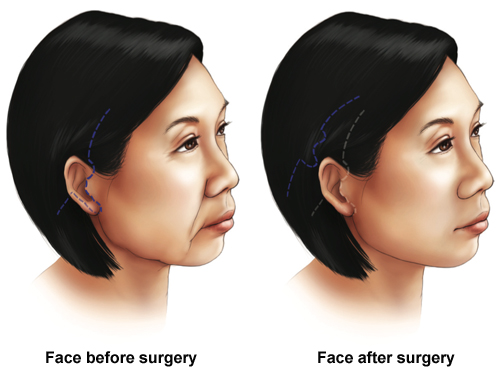
A rhytidectomy, or facelift, poses a risk of nerve injury, with the great auricular nerve being the most susceptible.
This nerve, crucial for outer ear and mastoid sensation, when affected, may result in numbness, difficulty with glasses or earphones, and occasionally, a painful neuroma.
Other facial nerves, particularly branches of the facial nerve governing muscle movement, can also be impacted, causing weakness or drooping in areas like the brow or lower eyelid.
Fortunately, most nerve injuries tend to self-heal within months. However, prompt consultation with your surgeon is imperative if you encounter numbness, weakness, or pain post-rhytidectomy.
Leave a Reply